The Gaming Blog
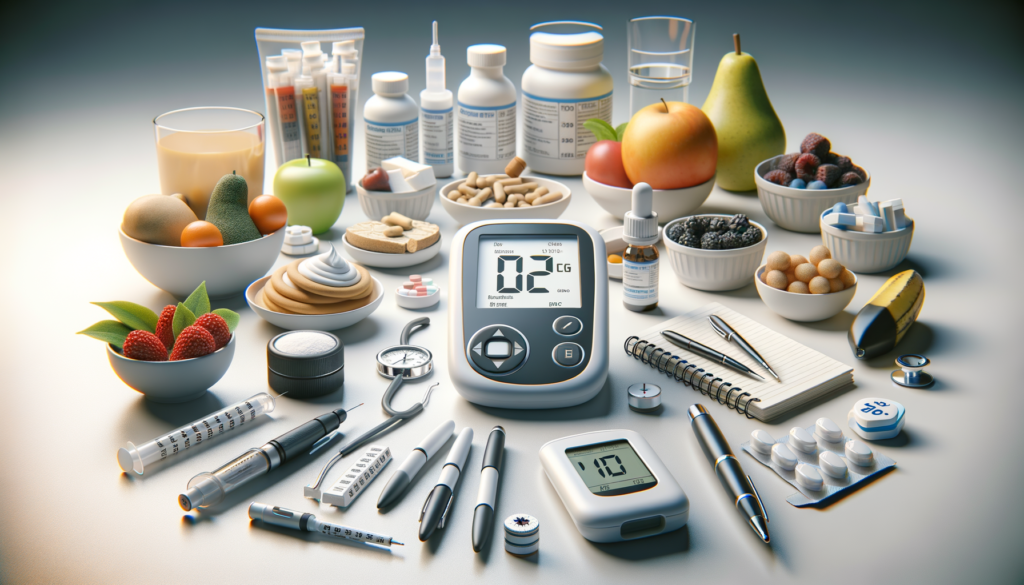
The Main Treatments for Diabetes
Lifestyle Interventions
Diabetes management often begins with lifestyle intervention, which is a cornerstone for controlling blood glucose levels and preventing complications. Dietary management is crucial, focusing on controlling total calorie intake and reducing refined sugar and high-fat foods. Increasing dietary fiber through whole grains and vegetables is recommended to delay sugar absorption. The DASH diet, which is low in sodium and high in fiber, not only helps in managing blood sugar but also effectively lowers blood pressure.
Exercise therapy is another vital component of lifestyle intervention. Engaging in at least 150 minutes of moderate-intensity exercise per week, such as brisk walking or swimming, can significantly improve insulin sensitivity and assist in weight control. Regular physical activity helps in maintaining a healthy weight, which is essential for diabetes management.
Drug Treatments
When lifestyle changes alone are insufficient, drug treatments become necessary. Oral hypoglycemic drugs are commonly used to manage diabetes. Biguanides, such as metformin, are first-line medications that reduce liver glucose output and improve insulin sensitivity. Sulfonylureas, like glimepiride, stimulate insulin secretion but may cause hypoglycemia, requiring careful monitoring.
Other oral medications include SGLT-2 inhibitors, such as dapagliflozin, which promote urinary glucose excretion and reduce cardiovascular risk. GLP-1 receptor agonists, like semaglutide, delay gastric emptying, promote insulin secretion, and aid in weight loss, offering a comprehensive approach to managing diabetes. Insulin therapy is essential for patients with Type 1 Diabetes (T1D) and advanced Type 2 Diabetes (T2D), with doses adjusted based on blood glucose monitoring.
Surgical Treatments
For some individuals with T2D, especially those with a Body Mass Index (BMI) of 35 or higher, metabolic surgery, such as gastric bypass, may be an option. This surgical intervention can significantly improve blood glucose control, and some patients may even achieve long-term remission. However, it requires long-term nutritional monitoring to prevent vitamin deficiencies.
Surgical treatments are not a universal solution but can be highly effective for those who meet specific criteria. The potential for diabetes remission post-surgery is promising, with some patients experiencing normal blood glucose levels without the need for hypoglycemic drugs.
Emerging Therapies
Research into emerging therapies offers hope for more effective diabetes management in the future. Stem cell therapy, still in the research stage, holds the potential to improve blood glucose control by repairing β-cell function. Precision medicine is another emerging field, tailoring treatments to individual genetic profiles for more effective management.
For instance, the combination of dapagliflozin and insulin for adolescent T1D patients has shown promise in reducing renal complications. These innovative approaches aim to provide more personalized and effective treatments for diabetes, potentially transforming how the condition is managed.
Diabetes Management and Complication Prevention
Effective diabetes management involves regular blood sugar monitoring, including fasting and postprandial blood sugar tests and HbA1c, with a target of less than 7%. Foot care is crucial in preventing diabetic foot complications, such as infections and ulcers. Vaccinations, like flu and pneumonia vaccines, are recommended to reduce the risk of infections.
Preventing complications is a key aspect of diabetes management, requiring a comprehensive approach that includes regular medical check-ups, adherence to treatment plans, and lifestyle modifications. By staying proactive and informed, individuals with diabetes can lead healthier lives and reduce the risk of complications.









